
The Duke Aging Center Postdoctoral Research Training Program (RTP) is housed at the Duke Center for the Study of Aging and Human Development (a.k.a. Duke Aging Center). The RTP provides comprehensive, multidisciplinary research training for both clinician and non-clinician scientists across the translational spectrum, equipping researchers with the skills and knowledge to drive innovation in biomedical, behavioral, social, and implementation science.
Funded by the National Institute on Aging (T32AG000029), the program offers 3 postdoctoral research training fellowship positions each academic year. Appointments are typically for a duration of two years, pending availability of funding and good standing in the program.
About the program
The overall goal of the Duke Aging Center T32 Postdoctoral Research Training Program (RTP) is to forge the development of independent investigators and leaders in the field of aging research, who are skilled in leading multidisciplinary, collaborative scientific teams that develop excellent, ethical science that benefits all segments of the older adult population.
Much of the training for each fellow is provided by that person’s faculty mentor(s) through a hands-on research apprenticeship program. A fellow carries out their research as a junior colleague in the mentor’s research program or laboratory. In addition, fellows attend a weekly interdisciplinary didactic seminar and other required didactics. The table below lists types of training activities and estimated time commitment for each.

A key component of the Duke Aging Center RTP is a weekly interdisciplinary seminar. Over a two-year period, its curriculum includes training in:
- research skills (e.g., team science, community and partner engagement)
- career development competencies (e.g., research dissemination, preparing and giving a job talk)
- core content areas in aging
- biomedical science
- behavioral science and neuroscience
- social science
- health services research/dissemination and implementation
This structure enables the RTP to provide highly specialized and individualized training in a fellow’s substantive area, while also providing a broad understanding of basic gerontological issues. This strategy encourages each developing scientist to relate their work to the overall field of aging, and, on a more practical level, to interact with other scholars and build a network of colleagues and collaborators in gerontology. The exchange of ideas that occurs in this interdisciplinary framework has, in fact, led to multidisciplinary work among fellows and faculty.
Our seminar is attended by the trainees from this and other training programs at Duke and in the area, by visiting scholars to the Aging Center and to the campus, and by faculty associated with the Aging Center. It is a forum for a discussion of gerontological issues from many perspectives.
 Nicole Arrato, PhD
Nicole Arrato, PhD
Dr. Nicole Arrato is a clinical health psychologist whose research lies at the intersection of psychology, oncology, and aging. Her program of research focuses on developing and evaluating behavioral interventions to reduce depression, anxiety, pain, fatigue, and other symptoms for older adults with cancer. Her T32 project is entitled, “Lung Cancer and Aging (LuCA): Intervention development for addressing aging-specific concerns in older adults with lung cancer.” This work is being conducted under the mentorship of Dr. Rebecca Shelby.
Nicole is originally from Connecticut. She completed her B.S. in Psychology at Fordham University, and her M.A. and Ph.D. in Clinical Psychology at The Ohio State University. She came to Duke University Medical Center for her psychology internship year and continued here for her postdoctoral training.
 Jacquelyn Coats, PhD
Jacquelyn Coats, PhD
Dr. Jacquelyn Coats is a Postdoctoral Research Fellow in the Aging Center at Duke University School of Medicine. Broadly, her research interests focus on the social determinants of health and aging for African Americans. Her current research centers on examining the health consequences of psychosocial stress, including discrimination, for older African American women’s health outcomes (cognitive, emotional, and physical). She also conducts research that seeks to identify the cultural assets and protective factors that buffer stress and facilitate healthy aging for African Americans across the life course.
Jacquelyn’s prior work experience includes serving as a program evaluator for community-based participatory research programs in St. Louis, MO and Detroit, MI, on projects aimed at reducing and preventing rates of chronic disease. She was also an Evaluation Fellow at the Centers for Disease Control and Prevention, where she supported evaluation of intimate partner and sexual violence prevention programs.
Jacquelyn earned her PhD in Social Work, Master of Social Work, and Master of Public Health all from Washington University in St. Louis and her Bachelor of Arts from the University of Michigan.
 Sam Honeycutt, PhD
Sam Honeycutt, PhD
Dr. Samuel Honeycutt is a cell biologist currently investigating the role of the immune system in ageing. He completed his undergraduate studies at the University of North Carolina at Wilmington (UNCW) and subsequently obtained his Doctorate in Cell Biology and Physiology from the University of North Carolina at Chapel Hill (UNC). Sam’s previous research has been multi-faceted and includes investigation into the role of the immune system in tissue regeneration, fate choices of hematopoietic stem cells, and the formation and patterning of blood vessels in the developing kidney. Currently, Sam is a post-doctoral Scholar in the lab of Dr. James White, where he is focused on the mechanisms of how immune cells can be utilized as a therapeutic approach to slow the aging process.
 Sid Madhavan, PhD
Sid Madhavan, PhD
Dr. Sid Madhavan is a clinical-translational scientist developing interventions for chronic diseases of aging. He graduated summa cum laude from Virginia Tech with a B.S. in honors in Clinical Neuroscience. He then completed his Ph.D. in Biology of Aging in a joint program between the University of Southern California and the Buck Institute for Research on Aging. During his doctoral research with Dr. John Newman at the Buck Institute, he identified how ketone bodies and other structurally-related metabolites can bind and clear damaged proteins within the brain.
At Duke, he is working in the labs of Dr. Laurie Sanders and Dr. Senthil Selvaraj on a diverse set of clinical trials spanning Parkinson’s disease and heart failure. The ultimate goal of his research is to develop therapeutic molecules which allow older adults to remain independent throughout the entirety of their lives.
 Tyler Reekes, PhD
Tyler Reekes, PhD
Dr. Tyler Reekes is a neuroscientist who investigates the neural mechanisms of vulnerability and resilience to postoperative delirium in older adults. He earned his undergraduate degree from Hampden-Sydney College and his Ph.D. in Pharmacology, Toxicology, and Neuroscience from Louisiana State University Health Sciences Center. His previous work examined the contributions to cognitive dysfunction in age-related neurodegenerative diseases such as Parkinson’s and Alzheimer’s disease. He is currently a Postdoctoral Scholar under the mentorship of Drs. Michael Devinney, Jeffrey Browndyke, and Miles Berger, where he studies how anesthesia and surgery act as a stress test for the aging brain to uncover why some older adults develop delirium after surgery while others remain resilient.
 Joab Odera, Ph.D.
Joab Odera, Ph.D.
Dr. Joab Odera is a Postdoctoral Research Fellow at the Duke Aging Center in the School of Medicine, working in the TORCHE Lab under the mentorship of Dr. Nosayaba Osazuwa-Peters and Dr. Katherine Ramos. His research integrates biostatistics, deep learning, and behavioral medicine to improve survivorship outcomes among older adults with cancer, particularly Head and Neck Cancer. Joab earned a B.Sc. in Molecular Biology from Winston-Salem State University and a Ph.D. in Integrated Biosciences from North Carolina Central University, where his research focused on metabolic reprogramming in alcohol-associated esophageal squamous cell carcinoma. He holds a certificate in Applied Data Science from MIT and additional training in Clinical Data Science from the University of Colorado. Joab has prior postdoctoral experience in non-small cell lung cancer research at the Duke Department of Medicine and completed the AIM-AHEAD Bridge2AI Clinical Care Training Program, which helped him apply his AI and ML expertise in clinical settings. His current work develops AI-enhanced tools for early detection of mental health vulnerabilities and personalized eCoaching systems to promote resilience and well-being. His long-term goal is to lead a research program that advances technology-driven interventions for aging populations.
Information for Applicants
- Interest and commitment to a career in aging research (interest in expanding expertise with multidisciplinary teams is preferred)
- US citizenship or permanent residence (green card holder)
- Doctoral degree/terminal degree in your field completed by the time to start the program (all coursework must be completed, and if applying for a PhD, final orals must be passed, and the dissertation signed before you can begin the program).
- At least two remaining years of post-doctoral training eligibility per NIH and Duke policy (see application form for details)
We will be recruiting three new post-doctoral fellows to begin in the Summer/Fall 2026.
The deadline to submit applications for this cycle is January 9, 2026. Selections will be finalized by April 2026.
To apply submit the following materials to AgingCenterRTP@duke.edu in a single PDF file.
- Candidate's current CV
- Candidate’s 2-page statement of interest (including research focus, training goals, and commitment to a career in aging research)
- Candidate’s graduate school transcripts (official copy)
- One Letter of Recommendation from a research mentor or faculty member from the doctoral degree program.
Basis for Judging Applications
Applications are assessed by a faculty committee via an NIH-style review and judged on the basis of their scientific merit, relevance to aging, and the fit of the trainee’s needs for training with the resources of the mentor and the training program.
Identifying a Mentor
The mentors listed below will be accepting post-doctoral fellows to start in the Summer/Fall 2026. Please review the list below and include the names of up to three potential mentors that fit your interests and goals for post-doctoral training in your completed Application Form. Feel free to reach out to specific mentors directly if you have questions about their research. For other questions about the Duke Aging Center T32 program, please contact AgingCenterRTP@duke.edu.
Our team is developing and validating brain MRI-based biomarkers of accelerated aging, especially in midlife, that can function as both risk indices for chronic age-related diseases and surrogate outcomes in randomized clinical trials of anti-aging interventions broadly as well as those targeting specific diseases. Ideally, postdoctoral trainees interested in joining our team will have a strong background in neuroimaging and geroscience.
Avshalom Caspi, Ph.D, and Terrie Moffitt, Ph.D.
Terrie E. Moffitt and Avshalom Caspi are recruiting a new postdoctoral fellow for fall 2026. We seek trainees who have a specific interest in midlife aging, its origins in early life, and its implications for mental and physical health in later life. The research training will be grounded in several large data sets where we map individual life histories (e.g., childhood adversity, environmental exposures, history of mental illness) onto changes in midlife brain structure, cognitive changes, epigenetic aging measures and risk markers for Alzheimer's disease and related dementias. Ideal candidates will have a strong background in programming and multivariate statistics.
Brian Andonian, MD, MHSc, ATC is a rheumatologist and clinician scientist studying the effects of exercise training, diet, and lifestyle interventions to improve immune health, joint health, and overall health for older persons with rheumatic disease, including rheumatoid arthritis (RA). The goal of his translational research is to improve outcomes in patients with chronic inflammatory diseases of aging such as RA, including disease activity, cardiometabolic risk, and disability, via personalized lifestyle prescription.
The Taylor lab uses molecular analyses, cellular studies, and mouse genetic modeling to study basic biochemical pathways of relevance to aging biology. Current projects focus on: (1) changes in fibrosis during tissue repair with aging, and (2) regulation of autophagy and mitochondrial homeostasis as relevant to immune function and inflammation.
The White Lab focuses on understanding molecular pathways altered with aging across tissues and utilize longevity interventions to inhibit or enhance such pathways to slow the aging process. We utilize human tissue, mouse and cell culture models in our approaches to investigate these topics.
We investigate how the microbiome shapes human health in aging. Our lab complements cutting-edge ‘omics technologies and computational tools with clinical studies, organoid platforms, and mouse models to investigate how the microbiome shapes epithelial and tissue-resident immune function in health and disease. Our current focuses include microbiome interactions primarily in the skin and respiratory tract, examining mechanisms of aging, infection, and antiviral immunity.
Dr. Johnson’s research focuses on reducing disparities in access to hospice and palliative care for older adults with serious illness. Fellows will have the opportunity to participate in various projects, including analyses of large secondary datasets related to advance care planning, qualitative data collection and analysis to understand factors related to disparities primary care related health outcomes, and other projects within the Health Disparities Research and Community Engagement Core of ASCENT (Advancing the Science of Palliative Care Across the Life Span), a national NIH-funded research consortium with a focus on improving outcomes for persons with serious illness and their caregivers.
The Sanders Lab is focused on understanding the etiology of neurodegenerative diseases, as well as biomarker and neurotherapeutic development. Dr. Sanders also designs and leads clinical trials for people with Parkinson’s disease and Alzheimer’s disease.
Dr. Marquine’s research focuses on addressing neurocognitive disparities in aging, with a focus on finding digital solutions to address these disparities. Fellows will have the opportunity to be engaged in various projects addressing neurocognitive disparities in Latino people at risk for Alzheimer’s disease and related dementias (ADRD), Parkinson’s disease, and HIV.
My laboratory investigates the neural correlates of memory and cognition in young and older adults using fMRI. We have three main lines of research: First, we distinguish the neural correlates of various episodic memory processes. For example, we have compared encoding vs. retrieval, item vs. source memory, recall vs. recognition, true vs. false memory, and emotional vs. nonemotional memory. We are particularly interested in the contribution of the prefrontal cortex (PFC) and medial temporal lobe (MTL) subregions and their interactions. Second, we investigate similarities and differences between the neural correlates of episodic memory and other memory and cognitive functions (working, semantic, implicit, and procedural memory; attention; perception, etc.).
Sarah Peskoe, PhD & Nrupen Bhavsar, Ph.D.
We lead an interdisciplinary program in study design and statistical methods to harness real‑world evidence (RWE), particularly EHR, claims, and registry data, to generate actionable insights for aging populations. Our research integrates data on the exposome and targets analytic problems that arise from heterogeneous routine clinical care, including informative missingness, time‑varying treatment patterns, and site‑level variation. Methodologically, we emphasize causal inference, transportability/generalizability, longitudinal modeling, and simulation‑based design evaluation, aiming to improve decision‑making for older adults with high comorbidity burden. Fellows will collaborate with clinical partners across Duke to co‑design studies, develop novel methods, and translate results for practice and policy. Ideal candidates bring strong skills in R/Python, experience with EHR data curation and quality assessment, and curiosity about how groups of people may age differently.
Tamara Somers, PhD, is a professor in the Department of Psychiatry and Behavioral Sciences and a clinical psychologist. Her research program focuses on the development, testing, and implementation of behavioral interventions for pain and symptom management in individuals with chronic illness. A central emphasis of this work is addressing the unique symptom management needs and challenges of older adults with multimorbidity (e.g., cancer co-occurring with arthritis). Trainees have opportunities to engage closely in ongoing NIH- and foundation-funded behavioral intervention studies; conduct secondary analyses using large, well-characterized datasets; leverage secondary findings as pilot data for grant submissions; receive structured training in grant writing with an emphasis on behavioral intervention development; and obtain mentorship and support in building an independent research program in symptom management in older adults.
The research focuses on developing extracellular vesicles (EVs) as biomarkers for aging, longevity, resilience, exercise response, and age-related diseases such as osteoarthritis (OA). The postdoctoral fellow could contribute to two major research directions:
(1) Identifying EV biomarkers and therapeutic targets for OA structural progression, in collaboration with Dr. Virginia Kraus
(2) Identifying EV biomarkers involved in metabolic health and exercise responsiveness, in collaboration with Dr. William Kraus
Stipend and Benefits
- Stipends will follow those set out by NIH and the Duke Postdoctoral Office for Postdoctoral Scholars.
- The program also provides health insurance (using the University’s insurance plan). For information on health insurance and other benefits at Duke, review the information provided by the Duke Postdoctoral Office.
- Partial travel support is provided when you are presenting your research at a professional meeting. If the proposed research will require additional funding, this should be discussed with your mentor.
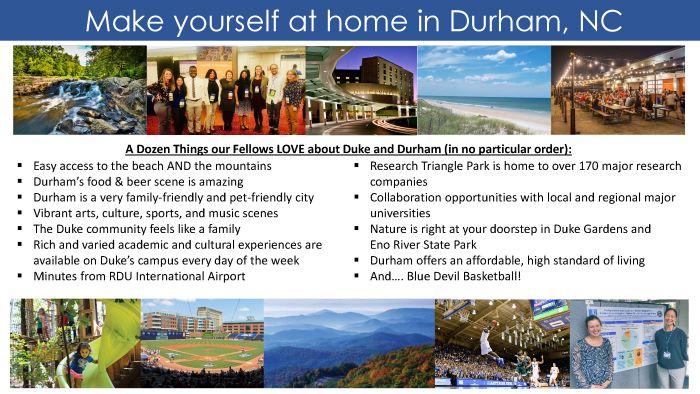
- Check out what Durham has to offer on the Discover Durham Website
- Explore the Duke School of Medicine's webpage
- Explore the Duke Aging Center webpage
- Take a virtual your of Duke's campuses
Postdoctoral appointees are an integral part of the research endeavor at Duke University. The Office of Postdoctoral Services (OPS) is the central resource for postdoctoral appointees on campus, and serves as a liaison between postdocs, faculty, administrators, and staff. The OPS promotes postdoctoral training at Duke and prepares Duke postdocs for successful careers both within and beyond academia.
People. Purpose. Progress.
The Office for Culture, Engagement, and Impact is committed to keeping human connection at the heart of institutional progress. We take actions that build and sustain an environment of inclusive excellence where everyone feels welcomed, valued, and empowered.
Bring people, ideas, and best practices together to inspire collaboration and elevate achievement among our faculty, staff, and students.
Advance strategic initiatives that reflect and uphold our shared values to positively shape our culture.
Drive accountability for the vitality of our people as central to our mission.
Office for Culture, Engagement, and Impact | Duke University School of Medicine

Questions?
If you have questions that are not answered by the content on this site, please contact us at AgingCenterRTP@duke.edu.